Chest & Back Pain on Exscortion With Heavy Beathing & Exteme Sweating
Overview
What is pulmonary hypertension (PH)?
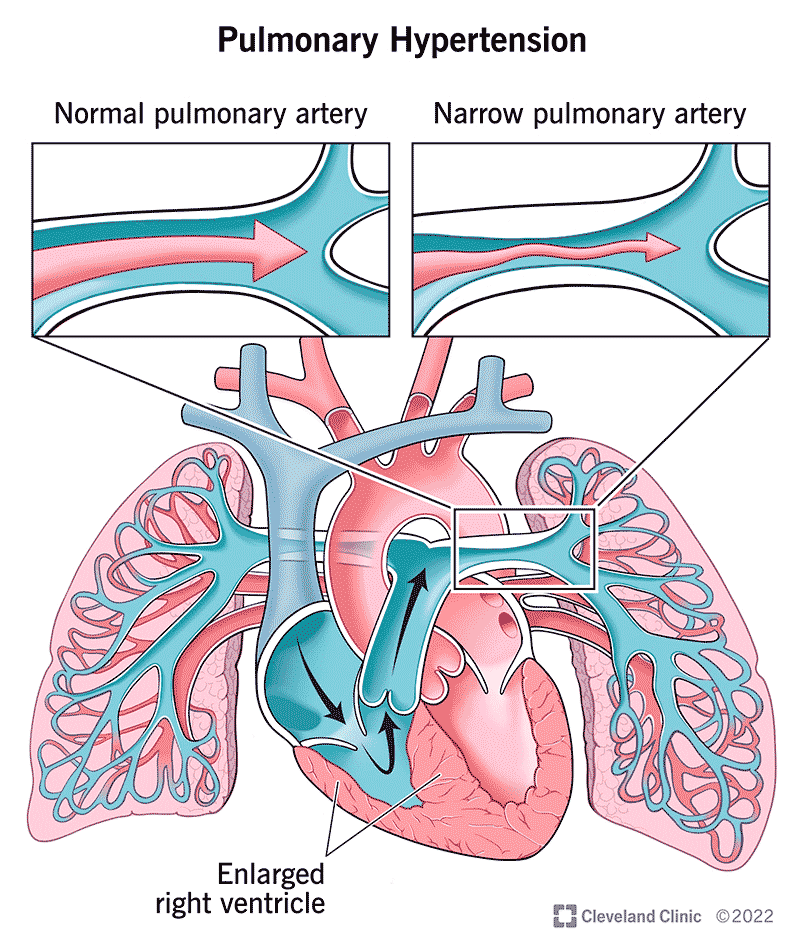
Pulmonary hypertension is a rare lung disorder in which the arteries that carry blood from the heart to the lungs become narrowed, making it difficult for blood to flow through the vessels. As a result, the blood pressure in these arteries -- called pulmonary arteries -- rises far above normal levels. This abnormally high pressure strains the right ventricle of the heart, causing it to expand in size. Overworked and enlarged, the right ventricle gradually becomes weaker and loses its ability to pump enough blood to the lungs. This could lead to the development of right heart failure.
PH occurs in individuals of all ages, races, and ethnic backgrounds, although it is much more common in young adults and is approximately twice as common in women as in men.
Why do the pulmonary arteries narrow?
Scientists believe that the process starts with injury to the layer of cells that line the small blood vessels of the lungs. This injury, which occurs for unknown reasons, may cause changes in the way these cells interact with the smooth muscle cells in the vessel wall. As a result, the smooth muscle contracts and grows more than is normal and narrows the vessel.
Symptoms and Causes
What causes pulmonary hypertension?
The following are some known causes of pulmonary hypertension:
- The diet drug "fen-phen." Although the appetite suppressant "fen-phen" (dexfenfluramine and phentermine) has been taken off the market, former fen-phen users have a 23-fold increase risk of developing pulmonary hypertension, possibly years later.
- Liver diseases, rheumatic disorders, lung conditions. Pulmonary hypertension also can occur as a result of other medical conditions, such as chronic liver disease and liver cirrhosis; rheumatic disorders such as scleroderma or systemic lupus erythematosus (lupus); and lung conditions, including tumors, emphysema, chronic obstructive pulmonary disease (COPD), and pulmonary fibrosis.
- Certain heart diseases. Heart diseases, including aortic valve disease, left heart failure, mitral valve disease, and congenital heart disease, can also cause pulmonary hypertension.
- Thromboembolic disease. A blood clot in a large pulmonary artery can result in the development of pulmonary hypertension.
- Low-oxygen conditions. High altitude living, obesity, and sleep apnea can also lead to the development of pulmonary hypertension.
- Genetics. Pulmonary hypertension is inherited in a small number of cases. Knowing that someone in the family had or has pulmonary hypertension should prompt you to seek early evaluation should symptoms occur.
Pulmonary hypertension may also be caused by other conditions, and in some cases, the cause is unknown.
What are the symptoms of pulmonary hypertension?
Symptoms of pulmonary hypertension do not usually occur until the condition has progressed. The first symptom of pulmonary hypertension is usually shortness of breath with everyday activities, such as climbing stairs. Fatigue, dizziness, and fainting spells also can be symptoms. Swelling in the ankles, abdomen or legs, bluish lips and skin, and chest pain may occur as strain on the heart increases. Symptoms range in severity and a given patient may not have all of the symptoms.
In more advanced stages of the disease, even minimal activity will produce some of the symptoms. Additional symptoms include:
- Irregular heartbeat (palpitations or strong, throbbing sensation)
- Racing pulse
- Passing out or dizziness
- Progressive shortness of breath during exercise or activity, and
- Difficulty breathing at rest
Eventually, it may become difficult to carry out any activities as the disease worsens.
Diagnosis and Tests
How is pulmonary hypertension (PH) diagnosed?
Because pulmonary hypertension may be caused by many medical conditions, a complete medical history, physical exam, and description of your symptoms are necessary to rule out other diseases and make the correct diagnosis. During the physical exam, your healthcare provider will:
- Listen for abnormal heart sounds, such as a loud pulmonic valve sound, a systolic murmur of tricuspid regurgitation, or a gallop due to ventricular failure.
- Examine the jugular vein in the neck for engorgement (enlargement).
- Examine the abdomen, legs, and ankles for fluid retention.
- Examine nail beds for bluish tint.
- Look for signs of other underlying diseases that might be causing pulmonary hypertension.
Other tests that might be ordered include:
- Blood tests:
- Complete metabolic panel (CMP): Examines liver and kidney function.
- Autoantibody blood tests, such as ANA, ESR, and others: Screens for collagen vascular diseases.
- Thyroid-stimulating hormone (TSH): A screen for thyroid problems.
- HIV: A screen for human immunodeficiency virus.
- Arterial blood gases (ABG): Determines the level of oxygen in arterial blood.
- Complete blood count (CBC): Tests for infection, elevated hemoglobin, and anemia.
- B-type natriuretic peptide (BNP): A marker for heart failure.
- Doppler echocardiogram: Uses sound waves to show the function of the right ventricle, measure blood flow through the heart valves, and then calculate the systolic pulmonary artery pressure.
- Chest X-ray: Shows an enlarged right ventricle and enlarged pulmonary arteries.
- 6-minute walk test: Determines exercise tolerance level and blood oxygen saturation level during exercise.
- Pulmonary function tests: Evaluates for other lung conditions, such as chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis, among others.
- Polysomnogram or overnight oximetry: Screens for sleep apnea (results in low oxygen levels at night).
- Right heart catheterization: Measures various heart pressures (i.e., inside the pulmonary arteries, coming from the right side of the heart), the rate at which the heart is able to pump blood, and finds any leaks between the right and left sides of the heart.
- Ventilation perfusion scan (V/Q scan): Looks for evidence of blood clots along the pathway to the lungs.
- Pulmonary angiogram: Looks for blood clot blockages in the pulmonary arteries.
- Chest CT scan: Looks for blood clots and other lung conditions that may be contributing to or making pulmonary hypertension worse.
Management and Treatment
How is pulmonary hypertension (PH) treated?
Appropriate diagnosis and analysis of the problem is necessary before starting any treatment. Treatment varies by patient, based on the different underlying causes, but generally includes:
- Taking medications
- Making lifestyle and dietary changes
- Having surgery, if necessary
- Seeing your doctor regularly
Listed below are medication, lifestyle and dietary suggestions, and surgical treatment approaches.
Medications
Many different types of medications are available to treat pulmonary hypertension. Treatment choices, such as those listed below, depend on the underlying cause of pulmonary hypertension, how severe the pulmonary hypertension is, how likely it is to progress, and a patient's drug tolerance.
- Oxygen — replaces the low oxygen in your blood.
- Anticoagulants or "blood thinners" such as warfarin sodium (Coumadin®) — decreases blood clot formation so blood flows more freely through blood vessels. Note: When taking anticoagulant medications, it is important for you to monitor bleeding complications and have regular lab work to monitor the level of medication in your bloodstream.
- Diuretics or "water pills" [such as furosemide (Lasix®), torsemide (Demadex®), spironolactone (Aldactone®)] — removes extra fluid from the tissues and bloodstream, which reduces swelling and makes breathing easier.
- Potassium (such as K-dur®) — replaces potassium (an essential nutrient) that may be lost with increased urination when taking diuretics.
- Inotropic agents (such as digoxin) — improves the heart's pumping ability.
- Vasodilators [such as nifedipine (Procardia®) or diltiazem (Cardizem®)] — lowers pulmonary blood pressure and may improve the pumping ability of the right side of the heart.
- Bosentan (Tracleer®), ambrisentan (Letairis®), macitentan (Opsumit) — helps block the action of endothelin, a substance that causes narrowing of lung blood vessels. Bosentan requires monthly lab work to monitor liver function.
- Epoprostenol (Veletri, Flolan®), treprostinil sodium (Remodulin®, Tyvaso®, Orenitram ® ), iloprost (Ventavis®) — dilates (widens) pulmonary arteries and helps prevent blood clots from forming.
- Sildenafil (Revatio®), tadalafil (Adcirca®) — relaxes pulmonary smooth muscle cells, which leads to dilation of the pulmonary arteries.
- Riociguat (Adempas®)
- Selexipag (Uptravi ®)
Medication guidelines
- Know the names of your medications and how they work. Keep a list with you.
- Take your medications at the same time every day. If you forget a dose, do not take two doses to make up for the dose you missed.
- Do not take any over-the-counter drugs unless you ask your doctor or pharmacist first. Some drugs such as decongestants (including Benadryl®, Dimetapp®, Sudafed® and other drugs containing ephedrine or pseudoephedrine) and nonsteroidal anti-inflammatory agents (such as Advil®, Motrin®, and Indocin®) can cause problems in people who have heart failure. Also avoid any over-the-counter medications whose labels state that caution is to be used if you have high blood pressure.
- Do not stop taking or change your medications unless you first talk with your doctor.
- Avoid herbal products because of their uncertain effects when combined with medications used for pulmonary hypertension.
Dietary changes
- Eat foods that are high in nutrients like potassium (e.g., dried fruits, bananas, oranges) and magnesium (e.g., peanuts, tofu, broccoli) and vitamins.
- Limit your total daily calories, if necessary, to achieve your ideal body weight.
- Limit foods that contain refined sugar, saturated fats, and cholesterol.
- Eat foods that are high in fiber, including whole grains, brans, fruits, and vegetables.
- Reduce your sodium intake:
- Buy foods that are low in sodium. Choose foods with labels that read "low salt" and "low sodium."
- Avoid table salt and seasoning salt.
- Avoid smoked, cured, salted, and canned meat products.
- Avoid fast food and limit prepared foods; they usually have a high sodium content.
- Monitor your fluid intake. Cut down intake of fluids if you have become more short of breath or if you notice swelling.
Lifestyle changes
- Monitor your weight: weigh yourself at the same time each day and record your weight in a diary or on a calendar. If you notice a rapid weight gain of 2 pounds in one day or 5 pounds over one week, inform your doctor.
- Lose weight if you are overweight (follow your doctor's recommendations).
- Have annual health check-ups with your primary care physician.
- Activity guidelines:
- Restrict lifting, pushing, or shoving to less than 20 pounds, since these activities increase the pressure in your arteries and lungs.
- Walking is important to keep your muscles strong and improve circulation. However, more strenuous forms of aerobic exercise should not be done regularly since your lungs may not be able to keep up with the oxygen demands placed on your body during these activities. Any activities that cause shortness of breath, dizziness, or chest pain should be stopped immediately. Contact your doctor if any of these symptoms occur.
- Do not smoke, vape or chew tobacco.
- Avoid or reduce alcohol intake.
- Avoid pregnancy; use contraceptives to prevent pregnancy.
- Maintain close contact with your healthcare providers.
Surgical therapies
- Pulmonary thromboendarterectomy : If present, blood clots in the pulmonary artery may be surgically removed to improve blood flow and lung function.
- Lung transplantation : Currently, this is the only cure for pulmonary hypertension that is caused by chronic blood clots. Transplantation is reserved for advanced pulmonary hypertension that does not respond to medical therapy. The right side of the heart will generally return to normal after the lung/lungs have been transplanted. About 1,000 lung transplants are performed every year in the United States. Many people are on the waiting list, yet a shortage of donors is the major limiting factor. Your healthcare provider will discuss transplantation if it is an appropriate treatment option for your condition.
- Heart/lung transplantation: This type of double organ transplant is very rare but is necessary for all patients who have combined lung and left heart failure.
Living With
When should I call my doctor about pulmonary hypertension (PH)?
Call your doctor if you are having problems with:
- Weight gain — 2 pounds in one day or 5 pounds in one week
- Swelling in your ankles, legs, or abdomen that has become worse
- Shortness of breath that has become worse, especially if you wake up short of breath
- Extreme fatigue or decreased tolerance for activity
- A respiratory infection or a cough that has become worse
- Fast heart rate (around 120 beats per minute)
- Episodes of chest pain or discomfort with exertion that are not relieved with rest
- Difficulty breathing with regular activities or at rest
- Restlessness, confusion
- Constant dizziness or lightheadedness
- Nausea or poor appetite
When should I go to the emergency department?
Go to the emergency department or call 9-1-1 if you are experiencing:
- Hickman catheter complications with intravenous prostacyclins, such as infection, catheter displacement/leakage of solution or blood, IV pump malfunction
- New chest pain or discomfort that is severe, unexpected, and is accompanied by shortness of breath, sweating, nausea, or weakness
- Fast, sustained heart rate (more than 120 to 150 beats per minute) — especially if you are short of breath
- Shortness of breath that is NOT relieved by rest
- Sudden weakness or paralysis in your arms or legs
- Sudden onset of severe headache
- Fainting spells with loss of consciousness
Resources
Where can I learn more about pulmonary hypertension (PH)?
To learn more about pulmonary hypertension, contact:
- Pulmonary Hypertension Association
801 Roeder Rd., Ste 100
Silver Spring, MD 20910
301.565.3004
Fax: 301.565.3994
www.phassociation.org - Cleveland Clinic Respiratory Institute
9500 Euclid Ave., A90
Cleveland, OH 44195
216.636.5327
Fax: 216.636.2054
https://my.clevelandclinic.org/departments/respiratory
Chest & Back Pain on Exscortion With Heavy Beathing & Exteme Sweating
Source: https://my.clevelandclinic.org/health/diseases/6530-pulmonary-hypertension-ph
0 Response to "Chest & Back Pain on Exscortion With Heavy Beathing & Exteme Sweating"
Post a Comment